
Fighting a pandemic is a joint effort; we cannot do it alone. Only if the majority of the community adheres to preventive behaviors, e.g., hand washing, social distancing, self-quarantining, can each individual person be safe. Thus, the COVID-19 pandemic shows characteristics of a social dilemma known as a public bad.
Back in May, when we started working together on Data versus Corona, few would have imagined that we’d celebrate New Year’s Eve at home, with less than a handful of people, in the midst of a new lockdown. While the majority of people adhere to social distancing guidelines, some ignored them, throwing large parties or travelling to distant relatives (see also here). From a psychological perspective, we can ask: what makes some people less likely to adhere to the guidelines?
With a team formed through Data versus Corona, we aimed to answer this question. While there were different people involved at different stages of the project, the core team consisted of Tim Draws, PhD candidate at TU Delft, Andrii Grygoryshyn and me (Clara Vetter), students at the UvA, and was coordinated by Caspar van Lissa, associate professor at Utrecht University. Needless to say that, in accordance with lockdown measures, all our communication went through Slack and video calls.
To gather data on psychological factors that may influence compliance with COVID-19 measures, we initiated a multi-country study investigating psychological factors that affect the spread of COVID-19. In the first phase of PsyCorona, cross-sectional data was collected during the first virus wave and the first lockdown between March and May 2020. The survey was translated from English into 30 languages by bilingual speakers. The assessed factors comprised demographics, personal factors that could affect an individual’s capacity to respond to the virus, social attitudes and norms, and virus-relevant personal concerns, values, and tendencies.
Before analyzing the data, we additionally added relevant publicly available country-level datasets to the individual PsyCorona data. These datasets included factors that could shape individual behavioural responses to the virus, falling in one of the following three categories: First, pandemic severity was indicated as the number of cases, deaths, and recovered patients (CSSE). Second, pandemic-related policies included both pre-existing and ongoing governmental responses to the pandemic. Third, pandemic preparedness included among others country-level ratings and health care resources. The whole analysis code and results have been publicly documented since the beginning of the project and are available on GitHub.
We used a random forest model which explained 52% of the variance in self-reported infection prevention behavior; the most predictive features are shown in Figure 1, which is from the preprint.
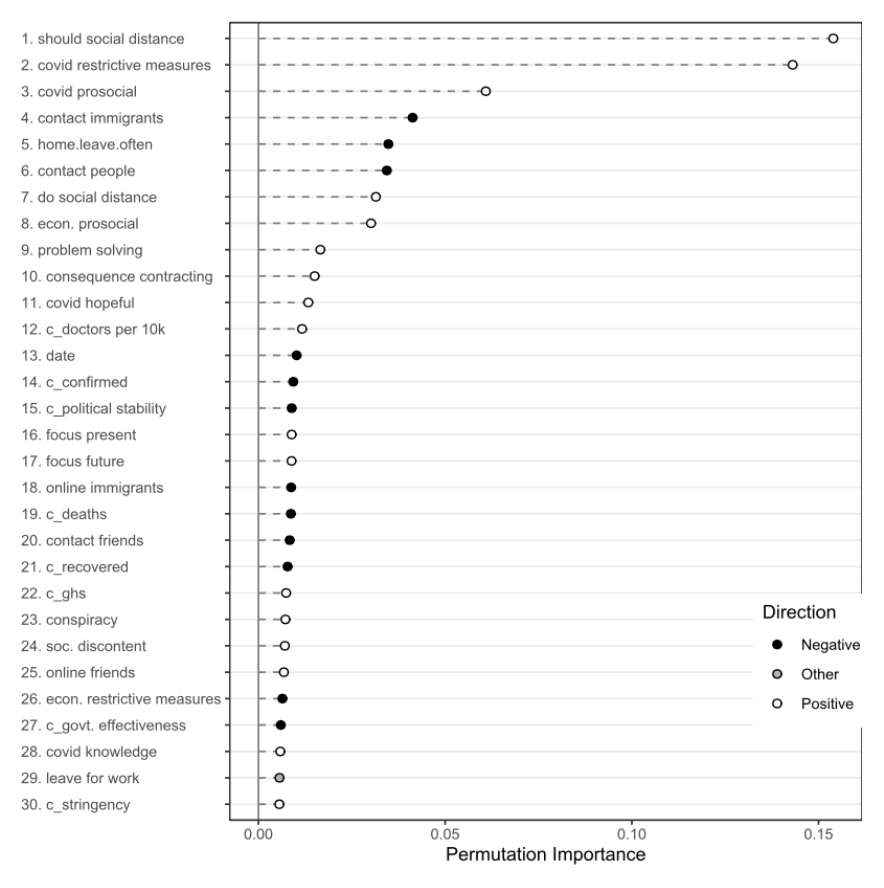
By far the most important indicators were individual-level beliefs and attitudes about how other people should behave, and how society should enforce infection prevention behavior. In fact, the two strongest predictors were the participants’ belief that one should adhere to the measures and their endorsement of extraordinary restrictive measures to contain the virus (including mandatory vaccination). These patterns suggest that people who are more likely to adhere intuitively perceive the prevention of COVID-19 infection as a social dilemma and understand that in order to overcome it we all have to cooperate. These patterns may also explain the tension between rule adherers and rule breakers in society.
The type of person who adheres to prevention behaviors is likely to have a problem-solving coping style, is optimistic, and willing to self-sacrifice to protect vulnerable groups. These qualities may present important psychological resources necessary to alleviate the costs of infection prevention measures, such as self-isolating, and to instead focus on the long-term goal. In terms of country-level predictors, individuals are more likely to comply in a society that has the political stability and health care infrastructure to take effective action to contain the virus and treat infected patients. For more details, take a look at the preprint available from https://psyarxiv.com/whjsb/.
